Procalcitonin-Guided Antibiotic Therapy: A Scientific Approach to Addressing Antimicrobial Resistance
Antibiotic resistance has become a major and imminent threat in today’s global public health. The World Health Organization (WHO) has identified antibiotic resistance as one of the most serious public health challenges of the 21st century. In this context, Procalcitoninn (PCT)-guided antibiotic treatment strategies stand out as a scientific solution to balance effective treatment with the reduction of unnecessary antibiotic use. This article will delve into the value, scientific rationale, and clinical application of PCT-guided antibiotic therapy, providing healthcare professionals with a practical tool to address the drug resistance crisis.
I. Antimicrobial Resistance: A Global Crisis That Cannot Be Ignored
Antibiotic resistance kills about 700,000 people globally each year, and it is projected that this number could climb to 10 million by 2050, surpassing the number of deaths from cancer, if effective measures are not taken. Overuse and misuse of antibiotics is a major contributor to the accelerated development of resistance. In many clinical scenarios, physicians are pressured by diagnostic uncertainty and are often inclined to use antibiotics “just in case”, especially in cases where bacterial infections are suspected but evidence is insufficient.
The current state of the clinic shows that up to 50% of antibiotic prescriptions may be unnecessary or inappropriate. This percentage is even higher in the treatment of respiratory infections. This overuse not only accelerates the emergence and spread of drug-resistant strains, but may also lead to microecological imbalances in patients, increased adverse drug reactions, and unnecessary healthcare expenditures.
II Procalcitonin: a biomarker revolution in infection management
Procalcitonin (PCT) is a peptide precursor consisting of 116 amino acids and is found at extremely low levels (<0.05 ng/mL) in healthy individuals. When a bacterial infection occurs, a variety of tissues and cells (including macrophages and adipocytes in the liver) produce PCT in large quantities in response to stimulation by pro-inflammatory cytokines, resulting in a rapid rise in serum concentration within 6-12 hours, with peaks of up to 1,000-fold or more.
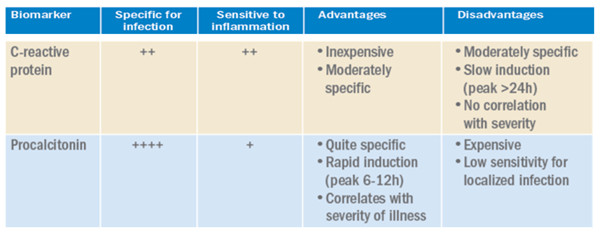
The biological properties of PCT make it an ideal marker for bacterial infection:
- High specificity: PCT levels are usually only mildly elevated or not elevated in virally infected individuals
- Rapid response: changes occur earlier than with traditional markers such as C-reactive protein (CRP).
- Moderate half-life: about 24 hours, reflecting changes in disease without excessive fluctuation
- Correlates with disease severity: PCT levels can help assess infection severity and prognosis.
Compared to CRP, PCT shows a clear advantage in differentiating between bacterial and non-bacterial infections. Studies have shown that PCT-guided therapy can reduce the duration of antibiotic use by approximately 30% without affecting clinical prognosis.
III Scientific evidence for PCT-guided antibiotic therapy
Over the past decade, several high-quality clinical studies have validated the effectiveness of PCT-guided strategies.The PROGRESS study, published in NEJM in 2017, showed that in critically ill patients, the duration of antibiotic therapy was significantly shorter in the PCT-guided group (7.5 days vs. 9.3 days), and there was no difference in 28-day mortality rates.A 2018 A 2018 meta-analysis that included 26 trials (total of 6,708 patients) concluded that PCT guidance reduces antibiotic exposure, decreases the risk of adverse events, and does not affect survival.
Clinical application scenarios include but are not limited to:
- Lower respiratory tract infections: help differentiate between bacterial and viral pneumonia
- Sepsis management: early recognition of bacterial infection and guidance for antibiotic initiation
- Postoperative infection surveillance: timely detection of infectious complications
- Acute exacerbation of chronic obstructive pulmonary disease: reducing unnecessary antibiotic use
- Neonatal sepsis: aid in early diagnosis
IV Specific Implementation Options for PCT-Guided Antibiotic Therapy
Effective PCT-guided therapy requires standardized clinical pathways. The following is a framework for an implementation program based on evidence-based medicine:
1. Initial assessment phase
- Detect baseline PCT levels when bacterial infection is suspected
- Combined with clinical symptoms, other laboratory tests and imaging results
2. Antibiotic initiation decision
- PCT ≥0.25-0.5 ng/mL: consider initiating antibiotic therapy
- PCT <0.25 ng/mL: strongly recommend withholding antibiotics and searching for other etiologies
- For patients at high risk of sepsis, thresholds may be appropriately lowered
3. Treatment monitoring and adjustment
- Monitor PCT trends daily
- PCT decrease ≥80% or absolute value <0.25 ng/mL: consider discontinuing antibiotics
- Persistent elevation of PCT: assess the possibility of treatment failure or complication.
4. Adjustment for special populations
- Patients with chronic kidney disease: interpret results with caution, may have slightly higher baseline levels
- Severe trauma/post major surgery: early elevations may not be due to infection
- Immunosuppressed patients: false-negative results may occur and need to be combined with other markers
V. Advances in PCT detection technology and quality control
Modern PCT detection technology has achieved high sensitivity and specificity. The current mainstream detection methods include:
- Electrochemiluminescence immunoassay (ECLIA): the lower limit of detection up to 0.02 ng/mL
- Fluorescence Immunochromatography (FIC): rapid (about 20 minutes), suitable for emergency care
- Enzyme-linked immunosorbent assay (ELISA): suitable for batch testing
To ensure the quality of the assay, the laboratory should:
- Establish appropriate reference intervals (usually <0.05 ng/mL is normal)
- Participate in external quality assessment programs
- Regularly calibrate instruments and monitor reagent stability
- Be aware of interfering factors (e.g., hyperlipidemic, hemolyzed specimens may affect results)
VI CHALLENGES AND SOLUTIONS IN CLINICAL PRACTICE
Despite the strong evidence, the promotion of PCT mentoring strategies faces a number of implementation barriers:
Physician perceptions and habits
Solution: Education and training to emphasize that PCT is an adjunct to, not a substitute for, clinical judgment.
Test accessibility and turnaround time
Solution: Promote rapid testing technologies and optimize laboratory processes.
Initial cost considerations
Solution: Balance the cost of testing by reducing antibiotic use and hospital length of stay
Risk of over-reliance on biomarkers
Solution: Emphasize that PCT results must be interpreted in the context of the clinical presentation.
VII Future Directions
The field of PCT-guided antibiotic therapy continues to evolve.
- Cutting-edge research directions include:
- AI-assisted analysis of PCT dynamic trends
- Combined application of PCT with other biomarkers (e.g. presepsin)
- Further optimization of rapid bedside testing techniques
- Exploration of potential value in antifungal treatment guidance
Conclusion
PCT-guided antibiotic therapy represents a paradigm shift toward precision infection management. Amid growing AMR threats, this approach equips clinicians to:
✔ Ensure timely treatment for true bacterial infections
✔ Avoid unnecessary antibiotic exposure
✔ Preserve long-term antibiotic efficacy
We urge healthcare systems to adopt this evidence-based strategy—aligning individualized care with public health priorities to combat one of our era’s greatest medical challenges.
By systematically implementing PCT-guided strategies, healthcare systems can significantly reduce antibiotic use without increasing risk, creating multiple values for patients and society – the perfect combination of precision medicine and public health safety that modern medicine seeks.
Post time: Jul-03-2025