Understanding Crohn’s Disease: Unveiling the “Green Cancer” and Its Scientific Detection Methods
Crohn’s disease is a chronic inflammatory bowel disease that has garnered significant attention in the field of digestive system diseases. Like an invisible fire dragon lurking in the digestive tract, its symptoms are subtle and varied, often posing significant diagnostic challenges. This article will provide a deeper understanding of Crohn’s disease and highlight how modern medicine, through precise diagnostic methods, can help patients navigate the complexities of diagnosis and treatment.
What is Crohn’s Disease?
Crohn’s disease is a chronic, relapsing, inflammatory bowel disease whose etiology is still unclear. Its most notable features are:
- Can Affect the Entire Digestive Tract:Inflammation can occur anywhere in the digestive tract, from the mouth to the anus, but the terminal ileum and colon are most commonly affected.
- Transmural Inflammation:Inflammation can penetrate the entire intestinal wall, causing not only intestinal symptoms but also potentially leading to deeper complications.
- Segmental Distribution:Diseased segments of the intestine alternate with normal, healthy segments, creating “skip” lesions.
Patients often suffer from abdominal pain, persistent diarrhea, weight loss, fatigue, and fever. Furthermore, it can lead to serious complications such as intestinal obstruction, fistulas, and abscesses, and even cause extraintestinal manifestations such as joints, skin, and eyes, seriously affecting quality of life.
Why is Precise Testing Crucial?
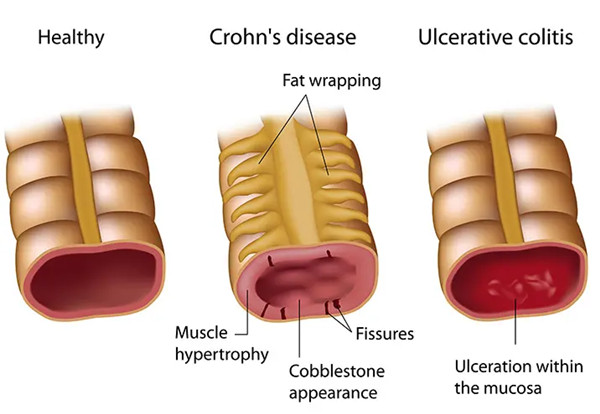
Because Crohn’s disease symptoms are very similar to those of many other intestinal diseases (such as irritable bowel syndrome, ulcerative colitis, and intestinal tuberculosis), misdiagnosis based solely on clinical symptoms is very easy. Therefore, a systematic and accurate testing program is the cornerstone for accurate diagnosis, disease assessment, and the development of personalized treatment strategies.
Unveiling the Core Detection Methods for Crohn’s Disease
The modern medical diagnosis of Crohn’s Disease typically follows a systematic, multi-dimensional verification process. As a professional medical testing institution, we offer the following key testing items:Modern medicine typically diagnoses Crohn’s disease using a multi-dimensional, step-by-step approach. As a professional medical testing organization, we offer the following key tests:
1. Preliminary Screening and Inflammation Assessment
1)Blood Tests:
- Inflammatory Markers: C-reactive protein (CRP) and Erythrocyte Sedimentation Rate (ESR) are sensitive indicators reflecting the level of inflammatory activity in the body; they are often elevated during active disease.
- Complete Blood Count (CBC):Can check for the presence of anemia (due to chronic blood loss or malabsorption) or an elevated white blood cell count (suggesting possible infection or inflammation).
2)Stool Tests:
- Fecal Calprotectin: This is currently a very important non-invasive biomarker. When intestinal inflammation occurs, neutrophils release calprotectin. Fecal calprotectin levels can effectively distinguish between Inflammatory Bowel Disease and functional disorders (like IBS), and can be used to monitor for disease relapse.
2. Endoscopy – The “Gold Standard” for Diagnosis
- Colonoscopy: This is the most important procedure for diagnosing Crohn’s disease. The doctor inserts a flexible tube with a camera through the anus to directly observe the mucosa of the colon and terminal ileum. If any abnormalities are detected during the examination, a biopsy is taken for pathological analysis. The presence of chronic inflammation and granulomas in the pathology report is decisive evidence for a confirmed Crohn’s disease diagnosis.
3. Imaging Examinations – Visualizing the Full Picture Inside and Outside the Intestinal Wall
While endoscopy visualizes the inside of the intestine, assessing the entire thickness of the intestinal wall for issues like thickening, narrowing, fistulas, or abdominal abscesses requires imaging techniques.
- Magnetic Resonance Enterography / CT Enterography:** These advanced imaging techniques can clearly display the morphology of the entire small intestine, accurately identifying transmural lesions such as wall thickening, strictures, and fistulas. They hold irreplaceable value for pre-surgical assessment and diagnosing complex cases.
4. Differential Diagnosis and Other Auxiliary Examinations
- Capsule endoscopy: For patients suspected of small bowel involvement but undiagnosed by other tests, capsule endoscopy acts as a “gut explorer,” capturing images of the entire small intestine and identifying early or hidden lesions.
- Pathogen testing: Stool culture or PCR testing is performed to rule out infectious enterocolitis such as Salmonella, Shigella, and Clostridium difficile, which can cause similar symptoms.
Conclusion
The diagnosis of Crohn’s Disease is a comprehensive process that often requires a combination of the various detection methods mentioned above. Early and accurate diagnosis is crucial for controlling disease progression and improving patient outcomes. At Xiamen Baysen Medical , relying on advanced testing platforms and a professional medical team, we are committed to providing clinicians and patients with accurate and reliable test results, working together to build a solid scientific foundation for overcoming Crohn’s Disease.
Post time: Oct-15-2025